How is the integration of artificial intelligence and machine learning in diagnostics and treatment planning revolutionizing patient care?
Zaineb Zouaoui
AIs are often portrayed as rogue robots with the goal of replacing mankind. What if we shift our view? As our world evolves at an unprecedented pace, the integration of AI and machine learning (ML) in healthcare is essential for further advancements in diagnostics and treatment planning. While the full potential of AI remains untapped, we face challenges such as privacy and legal concerns. However, by acting in accordance with the appropriate ethical boundaries, the potential of these technologies sets the stage for a transformative impact on patient care.
Nowadays, the idea of “patient-centred care” in the fields of medicine and allied health is coming more into view. What does that mean? And how can artificial intelligence help us uphold these values? Patient-centred care focuses on the patient and the individual's particular health care needs. The goal is to empower patients to become active participants in their care. Requiring the medical team to maintain good communication and address patient needs effectively. This also involves becoming a patient's advocate, aiming to provide effective and safe care.
ML involves educating a computer model using vast data sets to aid in building decision-making and predicting outcomes when presented with new patient data. This AI model can use various tests to rapidly consolidate information and provide highly accurate predictions. Firstly, a key benefit of integrating AI tools in healthcare is their ability to quickly analyze large volumes of medical data with the utmost precision, often surpassing human capabilities. This greatly improves workflow, leads to a faster diagnosis and, consequently, speedier treatment initiation.
AI is still in its early stages, not yet capable of being fully utilized for medical diagnoses. However, more data are emerging for the application of AI in diagnosing different diseases, namely, cancer. A study was published in the UK where authors input a large dataset of mammograms into an AI system for breast cancer diagnosis. Revealing that the interpretation of false positives and negatives was reduced by over 5%. Thinking on a larger scale, what can this bring in the future? It is evident that while still regularly going through its developmental stage, AI and ML have the capability to greatly reduce human error. In fact, according to author JM, Donaldson in “To Err is Human”, “a substantial body of evidence points to medical errors as a leading cause of death and injury,” specifically in the US. Greater precision in terms of diagnostic accuracy may, in fact, shift the worldwide demographic.
Another study was conducted in South Korea, where authors found that AI was more sensitive in diagnosing breast cancer with mass compared to radiologists, 90% vs. 78%, respectively. Similar techniques detected pneumonia from chest radiography, with a sensitivity and specificity of 96% and 64% compared to radiologists 50% and 73%. These statistics highlight that by identifying diseases earlier and more reliably, AI has the potential to deliver more personalized care and efficiently manage patient care. Most importantly, settings such as emergency departments, unfortunately, regularly face firsthand the rising burden of diseases and greater demand for time and health services. Fortunately, AI can assist in early and accurate disease detection, leaving space for timely interventions.
However, this raises the question: what does this mean for the future of this field? Will AI eventually replace doctors? Will we witness a drop in job opportunities for human clinicians? Or will this change shift responsibilities towards more complex, human-centred tasks?
As the workload and labour requirements of clinicians increased, the world is currently witnessing a significant global shortage of radiologists and pathologists, with the UK estimating a 40% shortage of radiologists by 2027. This remains a problem due to the growing demand for scans that require more time for interpretation. Luckily, as shown in the studies displayed above, it is clear that AI has the power to shift the medical field. In terms of delivering heightened accuracy, with a reduction in human errors and cost, as well as saving time (compared to more traditional methods). Likely, AI will soon be integrated into a doctor's day-to-day life. Possibly to support medical decisions and provide physicians with real-time guidance and assistance on the best course of treatment for patients. As a data-reliant mechanism, AI’s ability to provide quantitative measurements is essential to help identify abnormalities and detect other conditions. In addition, AI and ML aid in creating extremely tailored treatment planning options with high success prediction rates, based on family history, lifestyle, past medical records and more.
Evidently, “A study conducted by Huang et al. utilizing patients’ gene expression data for training a support ML algorithm, has shown to successfully achieve over 80% of prediction accuracy across multiple chemotherapy drugs.” “Another study performed by Sheu et al. demonstrated that antidepressant response could be accurately predicted with AI modelling. Demonstrating the promising role of AI, specifically in mental health. (Alowais, Shuroug A, et al. 22 Sept. 2023).
Ultimately, with all the possibilities within AI, it significantly impacts patient outcomes. Introducing higher success rates, more accurate disease detection, and faster treatment. Overall, these improvements reduce patient anxiety, enhance patient satisfaction and instill trust within the healthcare system over time.
AI can potentially unlock advanced tools, especially in underserved areas. Additionally, providing a more efficient and comfortable experience for the patient. While techniques are still being developed, this brings promising results in the improvement of patient care.
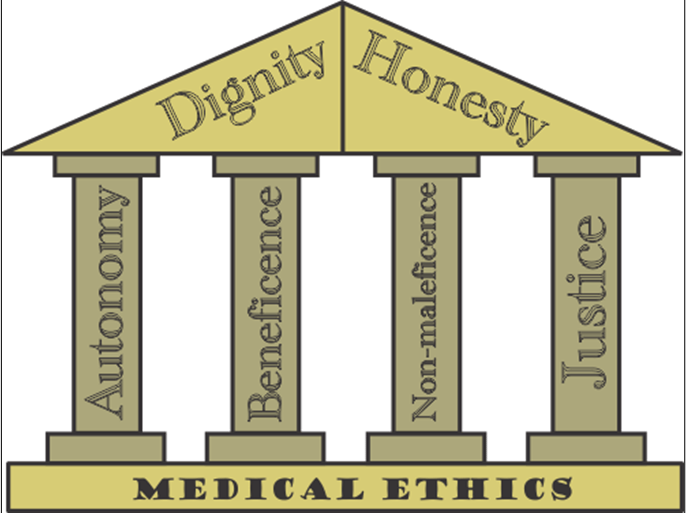
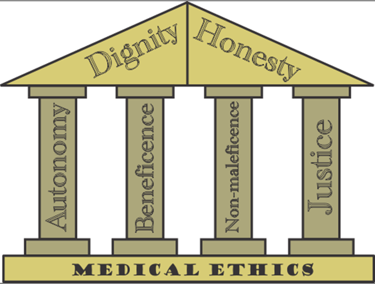
Figure 1: 4 pillars of medical ethics
Conversely, the benefits of implementing AI may not seem so black and white. AI will likely not be accessible in countries with limited resources. Its experimental nature and need for regular data may not be ideal for countries already scarce in medical resources. This widens the gap between countries, increasing inequality in access to the best patient care worldwide.
Additionally, AI lacks intuitive understanding, potentially leading to biases. Accountability, job loss, liability, and legal issues are all pertinent topics when discussing AI in healthcare. In this case, it is imperative to uphold the 4 main pillars of medical ethics (shown in the above, fig. 1). The implementation of such technologies without a doubt raises concerns about possible breaches to the patients' rights,
and may in fact violate non-maleficence (Do no harm…). As in most cases in medicine, there is never one straightforward answer when discussing such perplexing and complex ethical dilemmas. Rather, it is a case of my case scenario, where a doctor's judgment is in question. It is also for this reason that AI may never have the capability to replace the human mind. A lack of situational judgment proves that AI will continue merely as a tool for assistance.
However, what if the algorithms have made a misdiagnosis? Who takes the legal repercussions? One could argue that, seeing as the lead physician wasn't diligent and bluntly followed an unreliable algorithm, it's up to them. On the other hand, it falls upon the hospital to allow such experimental technologies. Could you blame AI? Again, one may argue that, of course, the lack of accurate diagnostic capabilities displays incompetence of the algorithm. Whereas another may counter that it lacks situational and initiative abilities, therefore, may not be questioned. If it isn't clear where I am getting at, this simply goes to show that there is never a clear case or a yes or no answer. We covered so many benefits within AI, and the capabilities it holds to transform healthcare worldwide. However, we remain frozen, dully struck by these ethical dilemmas and accountability concerns. Therefore, responsible authorities must formulate reliable regulatory frameworks for the ethical use of AI in healthcare.
In conclusion, AI and ML help us work more efficiently, reduce human errors, provide personalized treatments and revolutionize patient care. The pandemic caused massive stress on medical staff; hence, the integration of AI is crucial in helping us overcome future challenges. These endeavours are necessary, and we must work collaboratively alongside the proper frameworks to ensure the ethical use of AI.
Works Cited:
Ankur Tak, February 22, 2023, Artificial Intelligence and Machine Learning in Diagnostics and Treatment Planning. Journal of Artificial Intelligence & Cloud Computing, Vol. 2(1): 5-6, SRC/JAICC-162. DOI: doi.org/10.47363/JAICC/2023(2)150, accessed 31 Aug 2024
Asif Naveed, M, 31 May 2023, Transforming Healthcare through Artificial Intelligence and Machine Learning. Pakistan Journal of Health Sciences, 4(05). https://doi.org/10.54393/pjhs.v4i05.844, accessed 31 Aug 2024
David W. Bates, David Levine, Ania Syrowatka. et al. The potential of artificial intelligence to improve patient safety: a scoping review. npj Digit. Med. 4, 19 March 2021, https://doi.org/10.1038/s41746-021-00423-6, accessed 31 Aug 204
Petersson, Larsson, Nygren, J.M., et al. Challenges to implementing artificial intelligence in healthcare: a qualitative interview study with healthcare leaders in Sweden. BMC Health Serv Res, 01 July 2022, 850. https://doi.org/10.1186/s12913-022-08215-8, accessed 31 Aug 2024
Aamir Ali, et al. Exploring the current and prospective role of artificial intelligence in disease diagnosis. Ann Med Surg (Lond). 2024; 86(2):943-949. https://doi.org/10.1097/MS9.0000000000001700, accessed 31 Aug 2024
Shuroug Alowais, Alghamdi, S.S., Alsuhebany, N. et al. 'Revolutionizing healthcare: the role of artificial intelligence in clinical practice', BMC Med Educ, 22 Sep. 2023, vol. 23,1 689, https://doi.org/10.1186/s12909-023-04698-z, accessed 31 Aug 2024.
Navid Saidy, Artificial intelligence in healthcare: opportunities and challenges [online video], TEDx Talks, Nov 18, 2021, https://www.youtube.com/watch?v=uvqDTbusdUU, accessed 31 Aug 2024.
Revolutionizing Diagnostics, Treatment and Patient Care, [online video], UCLA Anderson, May 15, 2024, https://www.youtube.com/watch?v=p5c-fDHSjJo, accessed 31 Aug 2024.
Revolutionizing Healthcare: The Power of AI in Patient Care and Treatment [online video], Coach Tom, Dec 25, 2023, https://www.youtube.com/watch?v=KoIarX4Hdlg, accessed 31 Aug 2024
Byrne, Daniel W et al. “Artificial Intelligence for Improved Patient Outcomes-The Pragmatic Randomized Controlled Trial Is the Secret Sauce.” Korean Journal of radiology vol. 25,2 (Jan 10 2024): 123–125. https://doi.org/10.3348/kjr.2023.1016, accessed 31 Aug 2024
Harmon, Stephnie A et al. “Artificial intelligence at the intersection of pathology and radiology in prostate cancer.” Diagnostic and interventional radiology (Ankara, Turkey) vol. 25,3 (Apr 12 2019): 183–188. https://doi.org/10.5152/dir.2019.19125, accessed 31 Aug 2024
Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US); 2000. 2, Errors in Health Care: A Leading Cause of Death and Injury. Available from: https://www.ncbi.nlm.nih.gov/books/NBK225187/
Reynolds A. Patient-centred Care. Radiol Technol. 2009 Nov-Dec;81(2):133-47. PMID: 19901351.
